Epidermolysis bullosa (EB) refers to a group of rare, potentially-lethal, sometimes inherited conditions characterized by extremely fragile skin, which blisters and forms sores easily in response to minor trauma. EB shares similarities with other skin conditions such as dermatitis and psoriasis, which cannabis is known to benefit.
Due to the rarity of EB (approximately 19 per one million live births in the USA), there’s little existing research into the potential for cannabis to improve or possibly even cure EB. However, there is substantial evidence that shows how cannabis can aid some of the disease’s symptoms:
1. Using cannabis as an analgesic (pain management)
One almost-universal symptom of epidermolysis bullosa that cannabis may help to improve is chronic pain due to blistered and broken skin (as well as later complications such as loss, deformity, or fusion of fingers or toes). Various patient reports online testify to cannabis’ effectiveness in managing EB-related pain, and numerous physicians and dispensaries list EB pain as treatable with cannabis.
Research into chronic pain related to EB is non-existent, but a meta-analysis does support the finding that cannabis can help with chronic pain in general.
U.S. medical cannabis patient Miguel Garcia, who suffers from EB, has documented his use of cannabis to manage his symptoms. In fact he uploaded a YouTube video to explain how cannabis helped him “physically numb the pain” to the point where he didn’t even need to use opioid painkillers such as hydrocodone or oxycodone.

2. Cannabis can act as an antipruritic or anti-itch
Pruritus (itching) is another almost universal symptom of EB. There is a relatively wide selection of articles and papers available that attest to the fact that cannabis and certain synthetic cannabinoid analogues can act as antipruritics in cases of EB and several related conditions:
- In 2002, the synthetic agonist HU210 was shown to improve histamine-induced pruritus in atopic dermatitis.
- In 2012, a team of Japanese researchers (Odan et al.) discovered a synthetic CB2-receptor agonist that they named S-777469, and a dual CB1/CB2 agonist named S-444823, both of which significantly inhibited scratching without inducing psychoactivity.
- In 2005, it was shown that CB1- and CB2-receptors are present in the sensory nerve fibres and adnexal structures (appendages such as hair follicles and sebaceous glands) of the skin, and that they have an important role to play in the management of both itching and inflammation.

3. Taking advantage of cannabis’ anti-inflammatory properties
It’s hypothesized that inflammatory immune responses are the cause of blistering in many cases of EB. Cannabis has been shown to be effective against inflammation of the skin in numerous related conditions, and there are plenty of anecdotal reports of its effectiveness to be found online. The presence of dermal cannabinoid receptors is now thought to be crucial to the regulation of various immune responses, including regulation of oxidative stress and programmed cell death, as well as itching and inflammation.
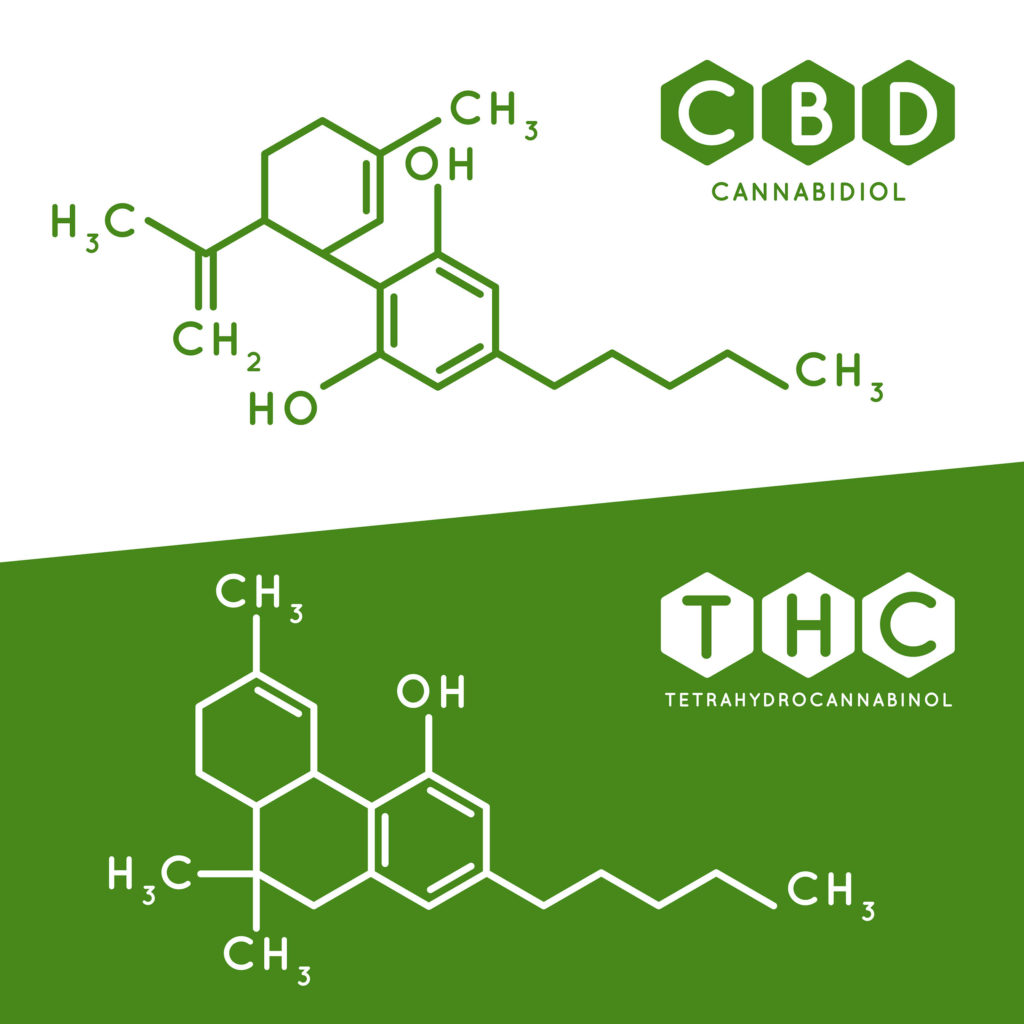
The mechanism via which cannabis exerts its anti-inflammatory effects is complex and not fully understood. It’s thought that both THC and CBD have anti-inflammatory properties, and that while the cannabinoid receptors are involved in the process, other mechanisms independent of the CB-receptors also have a part to play.
A 2013 study conducted by researchers at the University of Bonn in Germany demonstrated that both wild-type mice and CB-receptor knockout mice experienced improved dermatitis symptoms when administered topically-applied THC, indicating that the mechanism is CB-receptor independent.
However, there’s also evidence that CB-receptor agonists, such as THC or the endogenous agonist 2-AG, may induce dermal inflammation. This may be mediated by application of antagonists such as CBD. And conversely, there’s also evidence that 2-AG can inhibit inflammation via the CB2-receptor.
Thus, the precise relationship between endocannabinoids, the CB-receptors, and immune inflammatory responses in the skin is unclear, and gaining a clearer understanding of the mechanisms at work will allow us to develop targeted therapies to treat EB and numerous related conditions.

4. Help reduce infections by using cannabis as an antibacterial agent
A common complication of EB is infection due to exposure of broken skin to pathogens present in the natural environment. As well as causing pain to the patient, infected wounds prevent healing, may become necrotic, and ultimately contribute to all-round ill-health (as well as causing failure to thrive in children). The most common wound-colonizing bacteria in individuals with EB are staphylococcus, streptococcus, diphtheroids, pseudomonas, and candida.
Again, no specific research has been conducted on the ability of cannabis to combat bacterial infections in EB patients. But there’s abundant evidence indicating that it may exert a significant antibacterial effect in vitro and in vivo against various common bacteria and in the treatment of several important diseases.
Cannabis medications have been used as antimicrobials since the days of antiquity. In the late 19th and early 20th centuries, modern researchers began to document traditional folk uses of cannabis, and in many cases, demonstrate their veracity with new empirical methods.
In 1960, a landmark paper was published demonstrating the ability of cannabis extract to destroy several species of staphylococcus and streptococcus bacteria; since then, various other papers have found that cannabis can also kill pseudomonas and candida bacteria.
It’s clear that much work remains before we’ll have a complete understanding of the various ways in which cannabis can help this understudied disease. However, the existing evidence suggests that cannabis treatments could improve the symptoms of epidermolysis bullosa in several key ways, and that further research is needed.
- Disclaimer:This article is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your doctor or other licensed medical professional. Do not delay seeking medical advice or disregard medical advice due to something you have read on this website.










Thank you for sharing this valuable information.
I’m looking forward to learning more!
Peace,
CBD FOR ATHLETES
Sounds really good I want to try it on my daughter to suffers with RDEB,what dosage should she have and how does she take it etc..she’s 11 years old and suffers really bad every day.
Dear Lee
Thank you for your comment. We are sorry to hear about your situation. Unfortunately, as Sensi Seeds is not a medical or healthcare practice, we are not able to provide any advice relating to medical situations other than to consult your doctor or other licensed medical professional. This article, written specifically for healthcare providers who may not be aware of the many properties of cannabis, may be useful to you in talking with your doctor. You could also try to contact local medicinal cannabis support groups, if you have not already done so. In the UK, there is the United Patients Alliance (you can find them on Facebook) and in the US there are many branches of NORML (google NORML followed by your area name). We hope this is helpful.
With best wishes,
Scarlet
There was a story in local newspaper in Melbourne Australia about a little 12 yr. old girl sufferer of DEB. They would not print my comment to try Medical Marijuana/Cannabis oil. It is not yet legal here. It would also help my Rheumatoid arthritis as is has my USA/Canadian friends. Legalisation of medical cannabis goes before our Senate next week so hopefully will be legal soon.
As someone who suffers from this condition and a cannabis user it was fantastic to read this article. I have found using cannabis really helps with the pain and healing of my skin. Its sad that in England cannabis is still illegal and i’m treated as a criminal and discriminated against for choosing cannabis to help manage my condition, its ridiculous!