Cannabis use has been implicated in several cases of cerebrovascular accident (CVA) or stroke, and may also exacerbate cardiovascular ill-health that can lead to stroke in susceptible individuals. However, there’s also strong evidence that cannabinoid therapies may potentially assist in post-stroke recovery.
What is cerebrovascular accident?
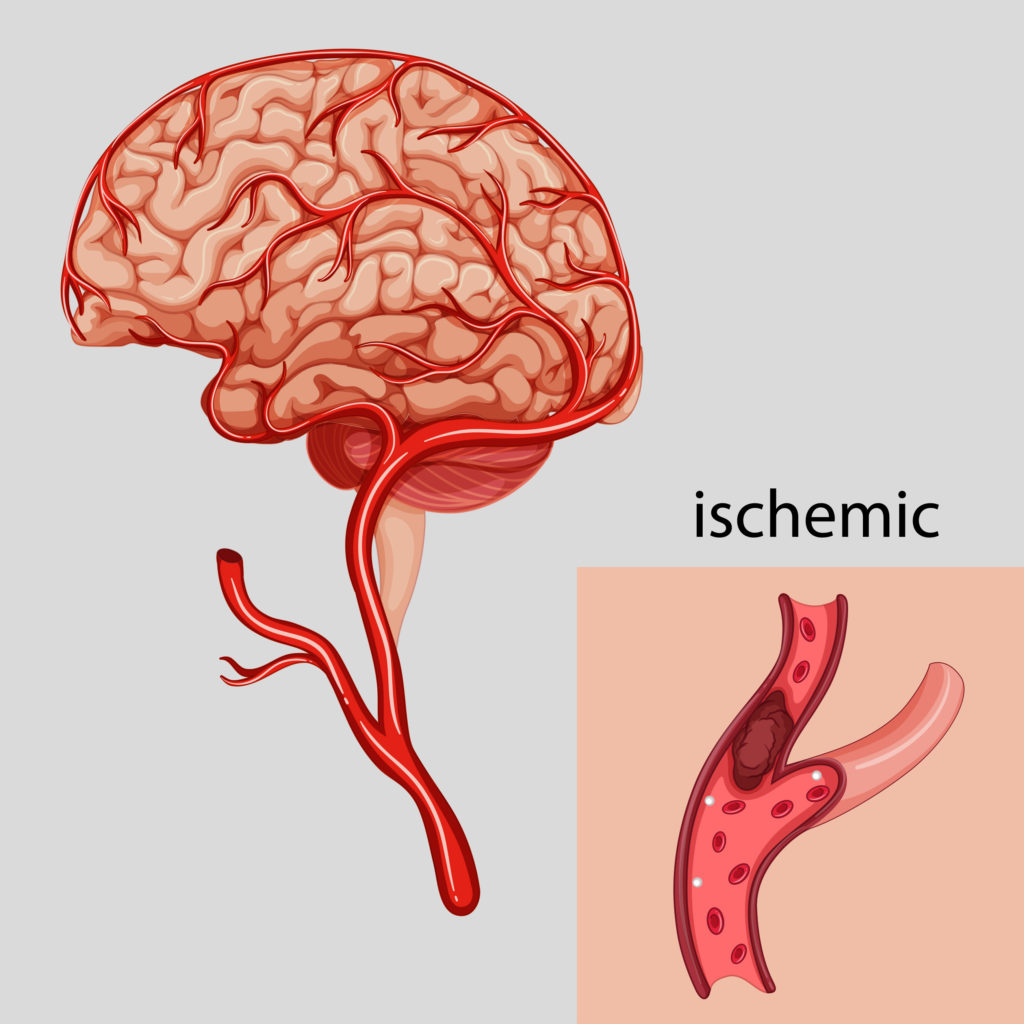
Cerebrovascular accident (CVA) is the formal term for stroke, an acute condition in which blood supply to the brain is interrupted or disturbed. Around 87% of all cases of stroke are ischemic in nature.
Ischemic stroke (IS) is caused by ischemia, or loss of blood flow, which in turn is usually caused by a blockage in the circulatory system such as an arterial embolism, atherosclerosis or thrombosis. Stroke may also be caused by haemorrhage of blood vessels in the brain—this is termed haemorrhagic stroke (HS).
As the blood flow (and therefore supply of oxygen) to affected regions of the brain is cut off during a stroke, the affected areas are unable to function as normal, and neurological and physiological functions related to them are disturbed or halted entirely. Depending on the length of time the blood flow is interrupted, this damage may be irreversible.
As our understanding of the field increases, we’re developing new and better therapies that can mitigate and reverse some of the effects of stroke. Cannabis and cannabinoid-based therapies are being rigorously assessed, due to their neuroprotective abilities.
Prevalence & risk factors
Stroke is a serious and debilitating condition that affects up to 15 million people worldwide every year and the number of sufferers continues to increase year-on-year. In the developing world, its prevalence is increasing as lifestyles become more westernised, while in the developed world, absolute prevalence is decreasing, but cases are still becoming more frequent as the population ages.
Stroke mostly affects those in the older demographic, and as our populations continue to age throughout the world, the burden on healthcare services is increasing. Aside from old age, other factors that predispose an individual to stroke include high blood pressure or cholesterol, diabetes, ischemic heart disease and tobacco use. High blood pressure (hypertension) is the factor most strongly associated with increased risk of stroke.
Evidence that cannabis use can increase the risk of stroke both in susceptible groups and in otherwise-healthy young adult males does exist, but a causal link has not yet been definitely established. Certainly, cases of stroke that can be linked to cannabis are a tiny fraction of the whole, but as cannabis use increases in many countries, we may see that tiny fraction increase.
Who’s more likely to increase risk of stroke with cannabis use?
Can weed cause a stroke? Most existing research into the subject indicates that very few people who use cannabis will experience an increased risk of stroke. However, a study from 2018 indicates that number is slightly on the rise.
Also, for those with certain underlying health conditions, cannabis use may increase the risk of stroke occurring—and may even directly trigger it in extremely rare cases.
Cannabis users suffering from ischemic heart disease, hypertension, and cerebrovascular disease may develop chest pain, cardiac arrhythmia, and (in extremely rare cases) acute myocardial infarction (MI). If an individual experiences MI, their risk of stroke is greatly elevated for the following month. A new study (2018) involving more than a million patients found that cannabis users who did suffer MI and were hospitalized, had a decreased risk of atrial fibrillation and in-hospital mortality compared to patients who didn’t use cannabis, but cannabis users were younger and were less likely to have known coronary disease prior to their hospitalization.
Patients with a cerebrovascular disease, such as atherosclerosis, may also experience strokes caused by cannabis-related changes in blood pressure.
The risk of symptoms occurring appears to be highest immediately following cannabis use, dropping to near-normal levels within thirty minutes. Because THC has analgesic effects it may mask chest pain, delaying treatment.
CVA and cardiovascular health
Cardiovascular disease is very strongly linked to risk of ischemic stroke. High blood pressure (hypertension) is often seen as a cardiovascular condition in and of itself, as it puts strain on the heart and can lead to various complications. It’s also a cause of many cardiovascular disorders. Hypertension is viewed as an independent risk factor, particularly if it is ‘primary’ hypertension and there’s no discernible underlying cause for its occurrence.
There are many other cardiovascular conditions that increase risk of stroke, including ischemic heart disease (progressive narrowing of the blood vessels supplying the heart), smoking, diabetes, brain aneurysms and personal or family history of any cerebrovascular disease (a group of diseases affecting blood vessels in and towards the brain, which include atherosclerosis and transient ischemic attack).
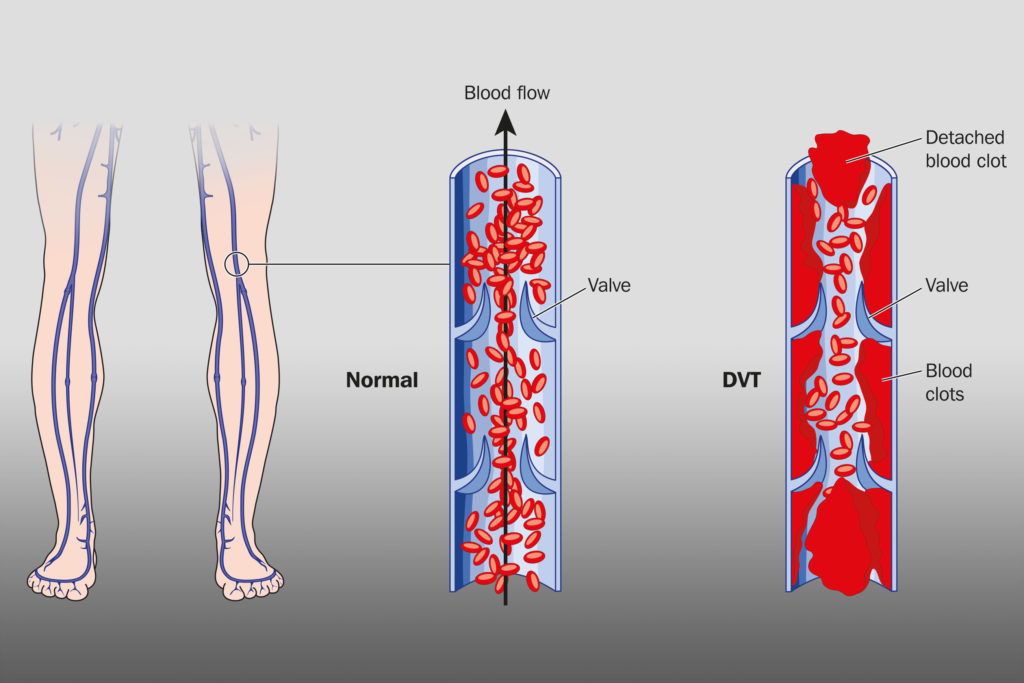
Thrombosis & embolism
Thrombosis and embolism are two other major factors, both of which involve obstruction to the blood vessels (thrombosis refers to blockages caused blood clots only and which occur at the site of origin, while an embolism may be a blood clot, a gas bubble or a globule of fat, and may occur in a part of the body that is remote from the point of origin). Around 30-40% of all ischemic strokes have no apparent underlying physiological cause; such instances are known as ‘cryptogenic’.
The endocannabinoid system, cardiovascular health and stroke
Various studies have theorised a link between cannabis use and acute myocardial infarction (MI). A study published in 2001 concluded that for a small subset of susceptible individuals, risk of heart attack increases by 4.8 times in the sixty minutes following use of cannabis. Individuals that suffer a heart attack have an increased risk of experiencing stroke during the thirty days following onset of MI.

Cannabis smoking increases the level of carboxyhaemoglobin in the blood, which decreases the rate of oxygen delivery to the heart, and increases blood pressure, thereby increasing the work of the heart. These side-effects are well-known to be associated with cannabis use. But the link between cannabis use and MI itself is not fully established, and is likely to only affect those in specific high-risk brackets.
CB1 and CB2 receptors are widely distributed within the cardiovascular system and play a role in modulating the cellular activity in the walls of the blood vessels. It’s been suggested that this mechanism may in some way contribute to the development of atherosclerosis, another major cause of ischemic stroke.
The CB-receptors, atherosclerosis & thrombosis
In atherosclerosis, the arterial walls typically begin to accumulate white blood cells, debris, cholesterol and fatty acids. These accumulations usually aggregate to form plaques known as atheroma. CB1 receptors have been found to express in certain white blood cells, known as macrophages, found within advanced atheroma.
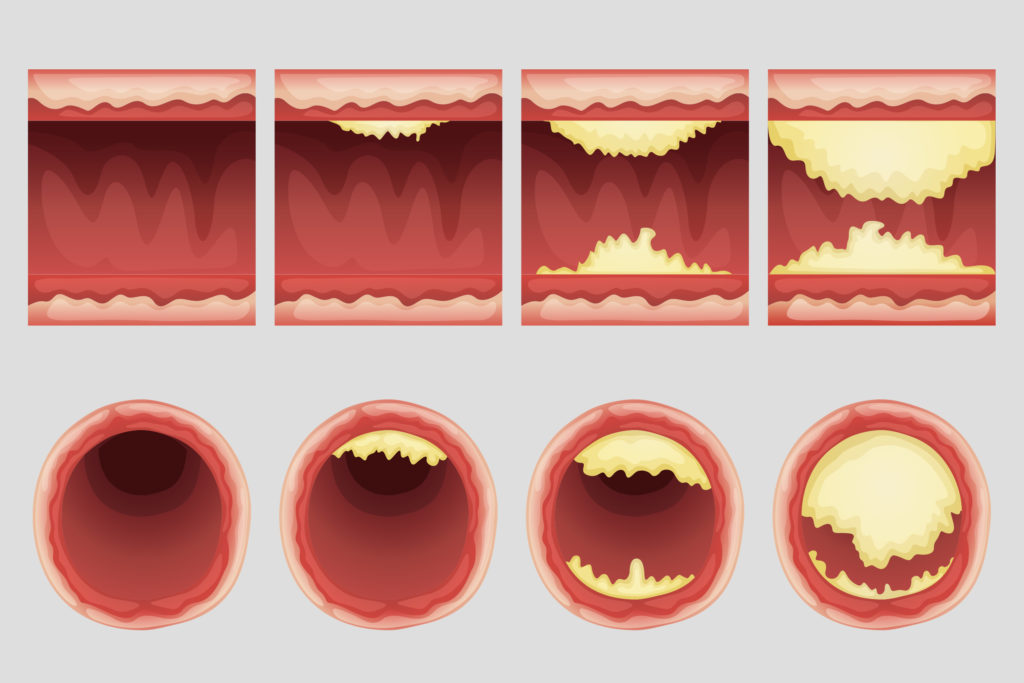
It’s not known what the precise mechanism at work is, but it’s been noted that patients with unstable angina (central chest pain due to ischemia of the heart) exhibit a markedly higher expression of CB1 and CB2-receptors in coronary arteries affected by atherosclerotic plaques than patients with stable angina.
The CB-receptor agonist delta-9 THC has also been shown to activate blood platelets via the CB-receptors, leading to increased expression of glycoprotein IIb/IIIa (a protein found in the platelets). A meta-analysis from 2012 suggested this in turn causes activation of factor VII, a protein that is strongly linked to thrombogenesis (growth of blood clots) by causing aggregation of the blood platelets.
However, it’s also important to recognize that that same meta-analysis described that other studies don’t come to the same conclusions, and might even suggest cannabinoids may inhibit platelet aggregation.
Cannabis arteritis and ischemic stroke
There have also been suggestions that cannabis can increase risk of stroke through a slightly different mechanism—the speculative disorder cannabis arteritis, which takes a form very similar to thromboangiitis obliterans (Also known as buerger’s disease, a known consequence of long-term tobacco use).
It’s thought that the recurrent inflammation of the blood vessels that characterises these diseases may occur in the brain as well as in the peripheral vessels, where it is more commonly found. If severe enough, these inflamed areas may cause obstruction of blood flow to the brain, leading to ischemic stroke.

However, it’s important to note that cannabis arteritis has not been conclusively demonstrated, and many of the studies that have investigated it have involved subjects that also used tobacco. Similarly, various studies and papers describe an association between cannabis and ischemic stroke, but many of these studies have been incomplete or flawed.
Cannabis implicated in cases of stroke
In New Zealand, a study into 218 individuals suffering from IS or transient ischemic attack, showed that twenty-five (15.6%) tested positive for cannabinoids in the urine, compared to just 8.1% of control participants. However, many of the participants also used tobacco. After adjusting for this, the researchers were unable to establish an association independent of tobacco.
In a review of medical literature conducted by Wolff, et al., 59 cases of stroke believed to be related to cannabis use were documented; 83% of these cases were ischemic stroke. The average age of the 59 individuals was 33 years, and men outnumbered women by almost five to one.
Studies have not proven an independent link
Cannabis use has been associated with an increased risk for stroke, but the absolute risk is likely small. Moreover, studies evaluating the association between cannabis and stroke tend to be limited due to recall bias, low risk cohorts, and other problems assessing exposure to cannabis. Nonetheless, many studies do indicate likely causality. For example, in a case study described by Wolff, of 17 IS patients who were exposed to marijuana justified a causal relationship by absence of other known risk factors, a temporal link between cannabis use and symptom onset, and the recurrence of symptoms with re-exposure to cannabis.
According to Wolff’s review, chronic users were more likely than occasional users to have experienced ischemic stroke. In many of the cases reported, stroke occurred during or within 30 minutes of cannabis consumption. A temporal association between cannabis consumption and IS was the main basis for suggesting a relationship.
Another review by Desbois and Cacoub documented 71 cases of cannabis users with IS. All patients were classified as heavy marijuana smokers. In 76.5% of the cases, symptoms again occurred during or within thirty minutes of consumption. While the temporal association is circumstantial, it does strongly point to cannabis’ ability to trigger stroke in specific cases. The other most notable piece of circumstantial evidence is the recurrence of symptoms on re-exposure.
THC, vasoconstriction and stenosis
It does appear that cannabis use may trigger stroke in rare cases, and there are various theories as to how this may occur. As well as potentially leading to development of atherosclerosis, presence of THC may trigger reversible cerebral vasoconstriction syndrome (RCVS). Several studies in animals and humans have shown that THC has peripheral vasoconstrictor properties.
Wolff reported the presence of multifocal intracranial stenosis (MIS) in 21% of cannabis users experiencing IS. This form of cerebral angiopathy, which manifests as severely narrowed cerebral arteries in multiple locations, was observed to reduce and ultimately disappear within three to six months following cessation of cannabis use
Desbois and Cacoub reported MIS in 50% of patients, RCVS in 43%, and single focus stenosis in 22.6%. A review of patients with RCVS reported an incidence of 32% for cannabis use; for almost half of those, cannabis was the only drug consumed.
Acute myocardial infarction & ischemic stroke
Cardioembolic ischemic stroke makes up 14-30% of all cases of IS, and in at least one case study has been associated with cannabis-related MI. Cardioembolic IS involves the occurrence of an embolism between the heart and brain, which causes a disruption of the cerebral supply and demand equilibrium, leading to stroke.
Given that the endocannabinoid system is linked so deeply with cardiovascular health, it’s likely that THC and other cannabinoids play a role in cardiovascular regulatory functions. In healthy individuals with no underlying condition or predisposition, the endocannabinoid could assist in maintaining good health. However, for those in high-risk groups, where the function of the cardiovascular system is already imbalanced, malfunctioning systems could cause adverse effects.
Beyond high-risk groups, there’s a small unexplained incidence of young, apparently-healthy individuals suffering from IS after cannabis use. It may be that there’s no link between these cases of stroke and cannabis use, or it may be that a genetic predisposition to such phenomena exists. Presently, the sole consistent variable found in patients with cannabis-associated IS is male gender.
More work is needed to establish the relationship
Evidence supporting the link between cannabis use and ischemic stroke is increasing, but a precise causal relationship is yet to be determined. The apparent chronological relationship between cannabis use and stroke onset is the most compelling circumstantial evidence. But relapses of IS with cannabis re-exposure also points to a causal relationship.
As medicinal cannabis becomes ever more available, and prescribed for an ever-increasing range of disorders, it’s is crucial that its potential side-effects are assessed. The side-effects of cannabis are apparently minor for the most part, and the subset of individuals that could potentially be affected is small. While it may not be justification to withhold cannabis medications from the wider population, the connection of cannabis to stroke should be considered when prescribed.
- Disclaimer:This article is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your doctor or other licensed medical professional. Do not delay seeking medical advice or disregard medical advice due to something you have read on this website.















There are incidents of cannabis-related cardiovascular events only if the dose prescribed has an imbalance of CBD: THC ratio i.e unregulated delta 9 THC component that is problematic. Recreational cannabis is detrimental and must not be confused with medical cannabis. THC is the main reason that raises oxidative stress and leads to cardiovascular or cerebral mitochondrial dysfunction. The issue lies within recreational cannabis such as Ghost OG, which has about 28% THC (Brucato,2019).
If used in edible form with overdose then it can lead to respiratory depression.
Such stroke incidents are frequent because of
1. Illicit access to recreational marijuana
2. increased perception that non-medical cannabis can heal 3.financial gains due to cannabis 3.widely accept impact of THC 5.youth being attracted to cannabis high in THC.
Hi Elena,
Thanks for your comment. Please could you provide links to evidence of your claims, so that we can further investigate them, and update our article if needed? Especially these sentences:
‘Recreational cannabis is detrimental and must not be confused with medical cannabis’; there is no difference between medical and recreational cannabis apart from the intention of the consumer – this article explains more about this increasingly common misconception.
‘If used in edible form with overdose then it can lead to respiratory depression’ – cannabis affects the endocannabinoid system, which does not include the parts of the brain responsible for respiration; this is why there has never been a death from cannabis use alone in the thousands of years that humans have been consuming it. The lethal dose for cannabis has been calculated at ‘ingestion of fifteen hundred pounds in fifteen minutes‘.
We have all our articles related to medicine and the medicinal use of cannabis checked by a medical doctor before they are published, as we take our role as a provider of information (as well as cannabis seeds!) very seriously.
With best wishes,
Scarlet
hans “pretty sure most of these stroke cases weren’t the most physically fit…” what a dumb arrogant silly comment. You demonstrate ignorance. You don’t know the difference between granulomatous arteritis and arteriosclerosis so you missed the entire point of the article. People prone to stenosis due to inflamatory processes are prone to vasoconstriction problems in particularly in the neck and head without pot and despite fit health. I have no body fat and I play drums an hour a day. Yet I’m not able to walk when I have a mini stroke, and I have them several times a day for the last twenty years. I bet I’m fitter than you
What are the main symptoms of your ministrokes?
I have been suffering from Hypertension for the last 3 years and I was totally unfit. One of my friends told me about PeaPlex is very helpful therefore.
I had a by pass in 2001, and I have hippertention I smoke about ten joint’s a day,
I feel fine feeling pretty good.
Should I stop now ia’m sixty three.
I smoked a lot in 2014 and I can confirm what people write. Sometimes when getting up or standing up I feel hits in my head. Very distracting on fitness clubs. I read that certain variations of herb cause such things. Stopped smoking and The condition gets better. I believe it was Kush not samica.
I personally would like to know if all these participants were tobacco smokers,their diet,whether they have histories in there families of heart disease etc.This study without the total case history of the ppl involved is bogus otherwise.Sounds like big pharm is trying to scare us here.
Smoking is injurious to health and can lead to higher risk of chronic hypertension. People who smoke regularly are more prone to heart related diseases.
Read the last sentence of the article.
Why weren’t women studied, too? Rhetorical question, really. Whatever the reason, it’s bullshit.
I am pretty sure most of those “stroke cases” those people weren’t the most physically fit I bet.
I have never gotten hypertrension from smoking weed until I took anti-psychotic drugs for a few months.
To Jacques the 53 yr old who’s smoked daily for 33yrs & all others: Sometimes to much of a good thing is NOT a good thing. Also from what I’ve come to learn about Cannabis and health is that smoking is not necessarily the best delivery when dealing with alleviating health concerns. A well prepared, non chemical solvent, decarboxylated oil(coconut oil apparently) seem to work well. And for some reason, in 2015 many still haven’t gotten the memo that when it comes to maintaining good health, diet(natural & organic as possible, meaning eliminate junk food, eat fresh produce not overcooked; mainly vegetarian – meaning less animal protein & fat; proper rest/sleep; regular exercise like walking etc, maintaining a sound, peaceful psychological/emotional well being-meaning- being in good accord with one’s self & others, knowing how to handle stress & knowing how to breathe slow & deep( proper breathing is more important than most know & most r not breathing properly); of course sufficient water consumption from a clean source, some recommend alkakine water (whatever sufficient is-some say 8 glasses. All I know we tend to NOT drink enough h2o), but at least filter most tap h2o to remove particulates & chlorine, flouride… Limiting alcohol use(as a society we consume to much damn alcohol! Oh but thats ok, but pot will kill ya right. SMDH), limiting the use & exposure if possible of the many environmental toxins we absorb one way or another every day
Add a good cannabis oil to above practices of a healthy lifestyle & stroke, heart attack and most other diseases & disorders should not be a factor. The Cannabinoids are most likely to be a benefit if health problems r an issue.
The reality is that we have a Endocannabinoid system(in our brains & throughout our bodies) that no one is talking about (thank you to Dr. Gupta
& others who are making the info available!). Otherwise for the most part it is not being addressed and most likely suffers deficiencies not being addressed. It’s not that cannabis is ineffective or causing cardiovascular & other health issues, it’s that we’re most likely using it in the wrong way and amounts and using it while carrying on with the same old bad lifestyle practices & habits. We’re the “take a pill” society who thinks taking a medication whether natural or synthetic, will cure us even as we continue those adverse to optimal health lifestyle practices.
It’s really a common sense thing: We(our bodies) have an Endocannabinoid system with cannabinoid receptors! The plant Cannabis has cannabinoids that synergistically link with those receptors in our bodies. Healing has been shown in many studies, over several decades, to occur when the two link. Add to that a US government patent on certain cannabinoids(who patents anything that’s ineffective?) now do the math while following the $$$$$! Just saying!
Hi i m 53 years old smoking cannabis for about 33 years on a daily base. I have been diagnosticed for arteritis and i i like to know if vaping or eating pot is safe for me? Any clues? Thanks jacques
just would like to say I had very serious stroke at the age of 55. Also aim an rn who working critical care I am also an occasional use of weed. The reason I had a stroke was a genetic problem called factor 5. The doctors told my family the stroke I had left people brain dead ! I survived regain all my mobility I was aphasia and had slight left side weakness I had great collateral circulation in my brain with kept blood flowing throughout my brain. Why? 2 weeks later when I got home I smoked a joint and could feel my brain light up much different than p stroke I say thank you marijuana!
lastly, have you noticed most of these studies come from France? Why aren’t we seeing this issue in western states like colorado and california
smoking has many toxic affects “If the THC caused the
> > alleged association or it was causal there would be research showing
> a
> > relationship to the oral consumption of cannabis and cannabinoids.
> > Also there has been substantial reseach that shows that cannabis is
> > nueroprotective, I do not find these anecdotal reports very
> > compelling.
from my cannabis dr “The bottom line is that there has never been a documented death from the use of any form of marijuana during recorded history.
The notion that marijuana causes strokes is absolutely ridiculous.
I quit smoking marijuana cold turkey and just had a stroke after 4-6 weeks without no wonder relapse is constantly recurring. I was in a study at the University of Washington up to 2002 , 15 years latter at the age of 60 I am having difficulties. Is there some one out there that can help? should I go back to Marijuana to avoid high blood pressure and any further stoke events?
Dear Suzanne
Thank you for your comment. We are sorry to hear about your situation. Unfortunately, as Sensi Seeds is not a medical practice, we are not able to provide any advice relating to medical situations other than to consult your doctor or other licensed medical professional. This article, written specifically for healthcare providers who may not be aware of the many properties of cannabis, may be useful to you in talking with your doctor. You could also try to contact local medicinal cannabis support groups, if you have not already done so. In the UK, there is the United Patients Alliance (you can find them on Facebook) and in the US and EU there are many branches of NORML (google NORML followed by your area name). We hope this is helpful.
With best wishes,
Scarlet
Please give more details about the studies cited, for example the Dr. Wolff study was searched ncbi database and found 59 cases, many associated with other drugs or predisposed conditions. Dr. Kloner new propaganda study mention cannabis being associated with hypertension and high calorie intake, but he didn’t mention that after eliminating tobacco use there was no association with hypertension and the cannabis user that used no other drugs had less diabetes and were less obese. When it comes to recurrent strokes we should see thousand, but with millions of people smoking cannabis daily, and the fact that smoking anything is toxic for the cardia system. I ask the topped dr. in the world in my opinion and this was a message from him on parts on your article.
i may not
> > have
> > > read this closely enough but these looked like relatively small
> > > numbers. There is no indication of how big a population we are
> > talking
> > > about.,how many used marijuana,when they last used it,what the
> > > incidence of stroke is in a matched sample for age,sex, and
> > > neighborhood. Without these facts and more, the results are
> pretty
> > > much meaningless. Also if this is related to THC we should see the
> > > same phenomenon with Marinol and Sativex and we don’t. Further
> the
> > > epidemiology should help us out. Was there an increase in stroke
> > with
> > > the high use of cannabis in the late 1960s and early 70s and a
> > > commensurate drop with the drop in marijuana use in the 1980s.
> > > This seems to be something that has caught your interest. There is
> a
> > > lot of work to be done to see if these results are real,are they
> > > reproducible,if they are real what is the mechanism of action.
> > > I’d call this alleged relationship to increased incidence of
> stroke,
> > > thin gruel.
> > > Frankly until I see that this same outcome of stroke is also
> > related
> > > to Sativex this is way on the back burner for me.There are many
> > other
> > > more pressing issues that I am looking into.
> > >
> > > good luck. if you find something other than this one study or
> > > something relating increased incident of stroke to Marinol or
> > > Sativex,let me know.
I just had a transitory eschemic attack just after I vaped. I’ve used cannabis since I was 18 (I’m 68). I’ve also been having frequent migraines for three months and I’ve suffered from depression since I was a teen. I’ve been taking SSRIs for 30 years. Don’t know what it all means, but it was very scary.
I was looking for reports on marinol, sativex, canabidol, animal studies, and dabs. There are no reports of RCVS, also RCVS is highly associated with depression and migraines which have been associated with self medicatings. Also, a study in brazil showed people with headaches have abnormal levels of cannabinoids. Sounds like endocannabinoid deficiency. Geller did a study showing acute cannabis use in teens called 100% of strokes in st. louis in 2004, obviously that study was wrong. We should see reports coming out of colorado but theres nothing and they are 47th when it comes to the strokes by state. Cannabis also seems to be an anti inflammatory. If it were the cannabinoids we should see people dying from dabs at remarkable level. 80% of schizo use tobacco but tobacco doesn’t cause schizo, Any Opinions?
Also a study this year showed no association and an inverse affect.
Only 59 cases in 20 years? we should see that daily if cannabinoid caused strokes. Self Medicating?
I just saw a bunch of old studies showing decrease in heart rate in long term users which can cause vasoconstriction. Other studies show vasodilation, do you grow a tolerance to that affect to, or does you heart rate decrease because vasodilation lets blood flow easier?
Hypertension occurs in approximately 8–10% of pregnancies.Most women with hypertension in pregnancy have pre-existing primary hypertension, but high blood pressure in pregnancy may be the first sign of pre-eclampsia, a serious condition of the second half of pregnancy and puerperium.