Rabies is a disease caused by the virus Lyssavirus rabies, which can infect all mammal species, including humans. Though there are vaccines, they aren’t readily available everywhere. Cannabis has been shown to help in some cases and may be something to consider for treatment, especially in these areas.
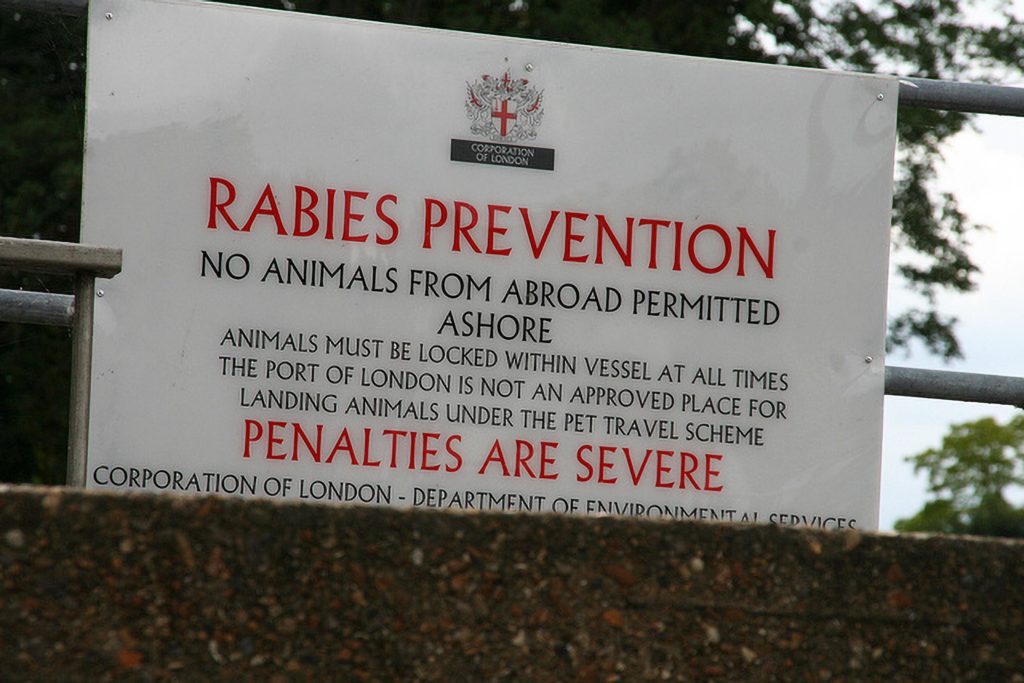
Although rabies isn’t easily transmitted between humans, around 60,000 fatalities occur annually around the world as a result of rabies each year with the vast majority (97%) being caused by bites from infected dogs. Most cases are in Africa and Asia.
How does rabies affect its host?
Rabies is an example of a non-contagious infectious disease. It can be transmitted between people and mammals (even those of different species), but relies on direct transmission of bodily fluids to be effective. Like the tetanus bacterium, the rabies virus is neurotropic, meaning that it preferentially attacks the nervous system.
The virus enters nerve or muscle cells immediately following the initial injury. It then ‘climbs’ up the synaptic junctions of the afferent nerves, from the peripheral nerve endings all the way up to the central nervous system (CNS). Once inside the CNS, the virus can cause acute encephalitis (inflammation of the brain), hydrophobia, muscle spasms and a range of other neurological symptoms.
Prior to the development of a vaccine (Pasteur & Roux, 1885), all cases of human rabies were fatal. Once a patient becomes symptomatic (which could take months), it’s still almost always fatal. In fact, rabies is the deadliest disease on earth with 99.9% mortality rate once symptomatic. However, unlike many other types of vaccines, today a rabies vaccine can be effective even after a bite has happened.
Alongside the various vaccines now in existence (both human and non-human), there are several treatment methods that have been successful against rabies, and the disease has been eradicated in several countries. Due to efficient post-exposure prophylaxis (PEP), which destroys the virus before it reaches the CNS, the mortality rate of rabies has been reduced.
History of cannabis as a rabies treatment
William B. O’Shaughnessy
Dr William B. O’Shaughnessy, the renowned ‘father’ of medical cannabis in Western medicine, was the first to document the use of cannabis as a treatment for rabies. He noted in 1843 that a symptomatic patient who later died experienced some relief from his symptoms after being administered with cannabis resin. This patient was even able to partake of small amounts of food and fruit juice, something that hydrophobia usually renders impossible in latter-stage rabies.
O’Shaughnessy observed that treatment with cannabis resin caused normalisation of the patient’s greatly elevated pulse rate, reduced spasms and perspiration, and calmed anxiety and excitation. It also allowed consumption of food and liquids. However, after four days of treatment the patient became comatose and died, although ‘without further struggle’.
John Ruxton, M.B.
In 1874, British Army Surgeon John Ruxton documented a case of a five-year-old boy who began to exhibit symptoms of rabies one month after being bitten by a dog. The disease had already reached an advanced stage, with the child experiencing severe convulsions, fever, delirium, and hydrophobia. But he treated the child with ‘a tincture of cannabis Indica’ and despite treatment being given so late, the child apparently made a full recovery after nine days.
After administration of cannabis tincture, the child would typically fall into a deep sleep and would awake with clear improvements to his condition. After the first dose, the delirium and convulsions were reduced. After the second, the child was able to ingest milk and broth, and after the third, he was free from symptoms, although he remained weak and drowsy. He was restored to full health over the course of the following week; four years later, he remained in good health.
Ruxton noted that use of cannabis was intended as a palliative measure only. He expressed his surprise at the child’s recovery to the extent of questioning his initial diagnosis, due to the rabies’ universal lethality at the time (just eleven years prior to introduction of the first vaccine).
The characteristic symptoms and case history strongly imply that the diagnosis of rabies was justified. However, it doesn’t appear that Ruxton’s success was replicated by others, and it’s apparently the only documented instance in which cannabis has caused a full recovery. Further research, utilising modern verifiable methods, would be needed to establish its true efficacy.
Could cannabis be effective against rabies?
Cannabis has been repeatedly demonstrated to be effective in management of muscular spasticity and convulsions. As a result, medicinal cannabis is now prescribed for various conditions that cause spasticity or convulsions, including multiple sclerosis, epilepsy and spinal cord injury.
There are also indications that cannabis may be useful in managing spasticity in Parkinson’s disease, cerebral palsy and amyotrophic lateral sclerosis (ALS; also known as motor neurone or Lou Gehrig’s disease). Cannabis appears to have some effect on all of these conditions, despite the fact that they occur via different means.
For example, ALS-related spasticity occurs as a result of lesions on the upper motor neurons, while MS-related spasticity occurs due to progressive disintegration of the myelin sheaths that surround the motor neurons. Of all known cannabinoids, cannabidiol in particular appears to exert an antispasmodic and anticonvulsant effect in both human and animal studies.
However, the complex mechanism at work is not yet fully understood.
The ‘Milwaukee Protocol’
The case of American teenager Jeanna Giese, who in 2004 survived rabies despite being unvaccinated, also throws up a potentially interesting possibility. Giese was put into a medically-induced coma before ketamine, midazolam, ribavirin, and amantadine were administered. This treatment (though with some later modifications) has since been dubbed the ‘Milwaukee Protocol’.
Treatment proceeded based on the doctors’ hypothesis that temporary brain dysfunction caused the detrimental effects of rabies. He theorized that if brain function could be slowed or halted temporarily, the immune system would have time to defeat the virus and the brain would be protected from damage.
The treatment was successful, although Giese was left unable to walk or balance and was forced to relearn.
Cannabis-induced stupor & coma
It may be the case that the ‘deep sleep’ experienced by the earlier mentioned boy treated by John Ruxton in 1874 was also responsible for the cessation of symptoms and subsequent recovery. Cannabis’ sedative and hypnotic effects are well-known, although whether it could slow brain function sufficiently for rabies to run its course without causing damage is unclear.
However, there’s some evidence that cannabis can indeed cause stupor—a state in which an individual is almost entirely immobile and unresponsive to stimuli—and even coma in young children.
In 2010, a 14-month-old child remained comatose for 48 hours following ingestion of cannabis. In this case, it was demonstrated that as levels of THC metabolite in urine declined, her prognosis improved.
In 2011, an 18-month-old child who fell into an unexplained coma was later found to have ingested cannabis.
In 2012, a 16-month-old infant became comatose following exposure to cannabis smoke. They detected THC levels in his urine and serum to be at 230 ng/ml and 112 ng/ml respectively, well over normal levels seen in passive cannabis smokers (50 & 30 ng/ml). After treatment with nasal oxygen and intravenous fluids, the infant made a full recovery.
In cases where it’s deemed necessary, coma is usually induced by administration of a barbiturate such as thiopental or pentobarbital, which slow cerebral blood flow and reduce metabolic rate of brain tissue. Cannabis use has been shown to reduce cerebral blood flow in inexperienced cannabis users significantly more than placebo, although overall metabolic changes may vary.
Could cannabis be part of rabies management programs?
In adults, it appears that cannabis can offer no more than palliative care. However, there’s some indication that medical cannabis may prove to be more effective in treating symptomatic rabies in children than in adults. It’s been shown to cause coma in children that is apparently reversible with no long-term ill effects, and which could potentially prevent rabies-related brain damage through its neuroprotective effect.
Although all demographics are susceptible to rabies, the disease is most common in children aged fifteen and younger; this age group also accounts for 40% of rabies-related deaths worldwide. Most cases of rabies now occur in Africa and Asia, regions that also produce abundant cannabis.
If low-cost treatments can be developed from cannabis, they may be highly advantageous in nations whose healthcare systems are not sufficiently developed to implement universal vaccination and post-exposure prophylaxis regimes.
In such countries, infected individuals will inevitably become symptomatic at higher rates; thus, establishment of cures rather than prophylactics is of far greater importance than in countries with the luxury of universal vaccination.
- Disclaimer:This article is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your doctor or other licensed medical professional. Do not delay seeking medical advice or disregard medical advice due to something you have read on this website.










I have used cannabis since 1973 to relieve severe muscle spasms resulting from a spinal cord injury in 1969. Very safe and effective for many medical conditions
Great article with an amazing explanation. And it is very clear and useful too. Thank you for sharing your great thoughts with us.
It’s good article…,,coz in Indonesia the goverment still make it ilegal,,there’s no research for the medicine..