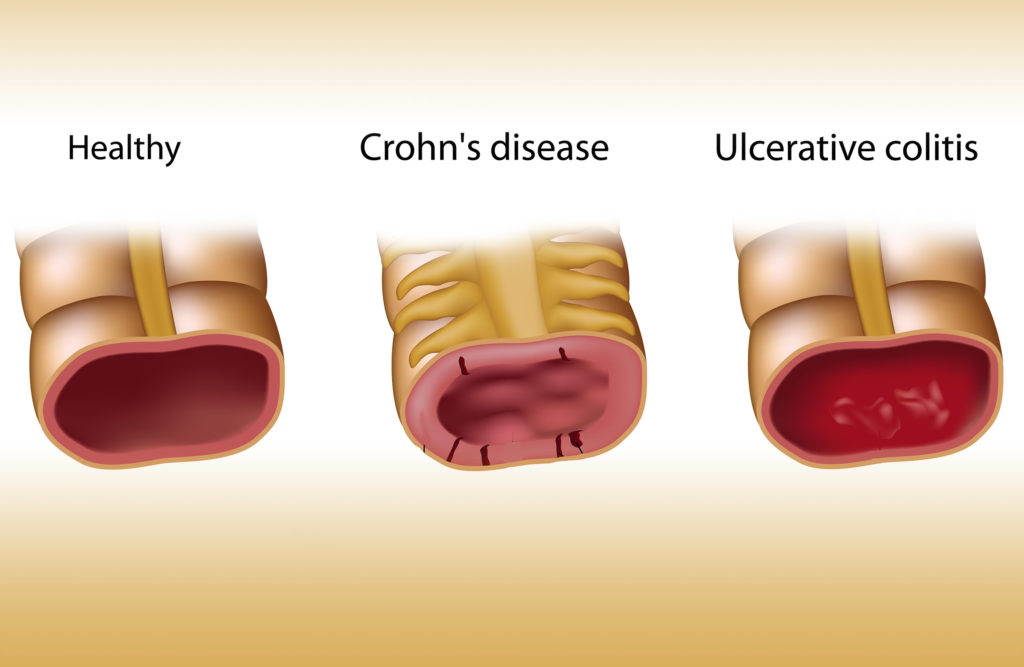
Inflammatory Bowel Disease (IBD) is an umbrella term for multiple different kinds of inflammatory bowel conditions, the most prevalent being Crohn’s Disease and Ulcerative Colitis. Conventional pharmaceutical medicine may lead to undesirable side effects, but cannabis may provide a less invasive form of treatment.
The prevalence of Inflammatory Bowel Disease remains elusive, as it is estimated that only 30% of those who experience symptoms of this condition will consult a physician. It is estimated that roughly 11% of the world’s population suffers an inflammatory bowel disease of some kind throughout their life.
Symptoms and causes of Inflammatory Bowel Disease
Symptoms are generally concentrated in the stomach, bowel, intestine and colon. Chronic diarrhoea, abdominal pain and cramping, unintentional weight loss, fatigue and fever are the most common symptoms associated with inflammatory bowel diseases. However, not all those diagnosed with this condition will experience all symptoms.
The cause of IBD is unknown, although most physicians speculate that genetics are a major factor. While diet and lifestyle play a crucial role in the management of symptoms, there is some scepticism about whether or not these factors are causally linked to the onset of the disease. The medical condition in question is inflammatory, which also suggests that a dysfunction of the immune system may be a causal factor.
Given that the condition is inflammatory, it is obvious why cannabis poses a potential line of treatment. Both THC and CBD exhibit potent anti-inflammatory properties. Plus, they target the endocannabinoid system, which is highly concentrated on immune cells and modulates immune function. Some researchers even hypothesize that at the root of inflammatory bowel diseases is an endocannabinoid dysfunction, putting cannabinoids in the limelight as treatment prospects.
IBD: Endocannabinoid deficiency, immune-mediated pathogenesis, or autoimmune condition?
As mentioned, the exact cause of inflammatory bowel disease is unknown. However, almost all scientific literature on the condition points towards some kind of immuno-related phenomena. While some researchers believe that IBD is a result of an underlying autoimmune condition, others suggest that some sort of immune dysfunction is at play, rather than specifically autoimmune. Another school of thought altogether, proposed by Dr Ethan Russo, is that treatment resistant GI disorders are caused by a clinical endocannabinoid deficiency (CECD).
The lack of understanding of what underlies IBD is probably the primary reason that it is so difficult to treat. Conventional pharmaceutical drugs for the treatment of IBD include corticosteroids and anti-inflammatory drugs, some of which have extremely undesirable side effects. Take Mesalamine, for example, which is the most common treatment for Ulcerative Colitis and Crohn’s Disease.
Patients with IBD usually tolerate this drug extremely well, but in some rarer cases, it can actually worsen symptoms and potentially lead to renal toxicity. This is where alternative therapies such as cannabis may have a significant role to play.
IBD’s strong link to immune dysfunction also makes cannabis a good candidate as a medicine for this condition. The CB2 receptors of the endocannabinoid system are highly concentrated on immune cells. Whether IBD is specifically an autoimmune condition or a dysfunction of the immune system, cannabinoids may have a positive role to play in modulating this response.
Otherwise, it is possible that CECD is the root of gastrointestinal diseases, as it has been shown that GI propulsion, secretion, and inflammation of the gut are all modulated by the endocannabinoid system. Targeting the endocannabinoid system rather than the immune system, according to this hypothesis, could reduce excess inflammation. With all hypotheses of the root of this disease in mind, there is a rationale for the treatment of IBD with cannabinoids.
The difference between IBD and IBS (Irritable Bowel Syndrome)
Although both IBD and IBS are related conditions, they are different in terms of both diagnosis and pathogenesis. IBD is an inflammatory condition that is most commonly associated with immune dysfunction. IBS, on the other hand, is not necessarily inflammatory, but is often associated with psychological factors.

Many of the symptoms of IBD and IBS are the same, including abdominal cramping and diarrhoea. However, unlike IBD, IBS is not associated with inflammation of the colon and intestines. Because the two conditions share many symptoms, cannabis may also have a role to play in treating IBS symptoms. However, there is very little scientific literature on this topic.
Exogenous and endogenous cannabinoids for the regulation of intestinal inflammation
The endocannabinoid system has homeostatic effects on intestinal inflammation, and this has been demonstrated in multiple studies. The effect of endogenous cannabinoids and their degradation on inflammation of the gut and intestines demonstrates a pathway through which exogenous cannabinoids can be medically applied.
For example, in this 2004 study, researchers investigated the role of CB receptors in the treatment of mice with induced colitis. The researchers noted stronger inflammation in mice with a CB1 receptor deficiency. When the mice were treated with a CB antagonist, the mice expressed symptoms similar to those with a CB receptor deficiency. Mice that were treated with a CB agonist showed increased protection against the induced colitis. The results of this study suggest an enhancement of endocannabinoid signalling during colitis.
In another rodent study conducted in 2014, researchers administered FAAH inhibitor, PF-3485 to mice with TBNS-induced colitis. The FAAH inhibitor reduced the induced colitis and demonstrated anti-inflammatory qualities linked with altering the levels of certain biolipids. Another study used MAGL inhibitors and observed the same result. The link to the endocannabinoid system is here: FAAH is the enzyme responsible for the degradation of anandamide, while MAGL is the enzyme responsible for the degradation of 2-AG. These are both endogenous cannabinoids of the endocannabinoid system.
The research suggests that increasing endogenous cannabinoid levels may protect a person against colitis, or halt the progression of the disease. At the very least, the scientific community is aware that CBD behaves as an FAAH inhibitor. This is just one example of how exogenous cannabinoids may be able to elicit the desired response from the endocannabinoid system. In any case, the scientific literature demonstrates a strong link between the endocannabinoid system and gastrointestinal inflammation.
Clinical trials and scientific research into cannabis and IBD
One of the first European medical applications for cannabis was the treatment of stomach pain related to cholera, and was brought to Europe from India by Sir William Brooke O’Shaughnessy. Unfortunately, the nearly-100 year period of prohibition means that modern science is only just beginning to catch up with the theories and observations of the past. Nonetheless, some scientific evidence points towards the efficacy of cannabis for certain symptoms related to IBD.

In one questionnaire that included 292 patients with IBD, almost 52% had used cannabis at some point during their illness to manage symptoms. Of them, 16.4% said they used cannabis to treat their medical symptoms, most of which were related to abdominal pain. This indicates a significant number of people self-medicating with cannabis.
In another questionnaire style cohort study, 313 patients with IBD were examined. Of them, 17.6% used cannabis to relieve symptoms related with IBD. The patients who used cannabis reported an improvement in abdominal pain (83.9%), abdominal cramping (76.8%), joint pain (48.2%) and diarrhoea (28.6%). However, this study also noted a higher risk of surgery requirements in those who used cannabis for 6 months or longer.
The Israeli Medical Association also conducted an observational study on 30 patients suffering from Crohn’s Disease (a form of IBD). Of 30 patients, 21 significantly improved after treatment with cannabis. The need for other forms of medicine was also significantly reduced. In contrast to the previous questionnaire, researchers observed a lesser occurrence of surgery in those who used cannabis.
Finally, a small randomized, placebo-controlled clinical trial for the effect of cannabis on patients with Crohn’s was published in 2013 in Clinical Gastroenterology and Hepatology. It was the first prospective and controlled clinical trial on THC for Crohn’s Disease. In total, 21 patients were included in the study who had not responded to therapy with steroids, immunomodulators, or anti-tumour necrosis factor-α. Patients in the cannabis group were given cannabis twice daily, in the form of cannabis cigarettes containing 115mg THC. The placebo group received cannabis flowers from which the THC had been extracted.
Complete remission was achieved by 5 of the 11 subjects in the cannabis group and 1 of 10 subjects in the placebo group. Three patients in the cannabis group were also weaned from steroid dependency. The researchers admit extreme promise for THC treatment of Crohn’s, although further studies with larger patient groups are required.
Cannabis for the management of IBD-related symptoms
It is possible that IBD patients self-medicate with cannabis as a way to manage some of the symptoms rather than targeting the actual cause of the disease. Many of the symptoms associated with IBD can be managed by cannabinoids, and while they may not pose a cure by any means, they may assist in the management of pain and inflammation.
Both THC and CBD have demonstrated potent anti-inflammatory and analgesic qualities. The two often come hand in hand, as inflammation of the gut in IBD is usually the cause of pain. Management of pain is a crucial factor in those who have IBD, as this symptom can be debilitating. Intraperitoneal CBD treatment on mice has also been shown to improve symptoms of colitis such as colonic inflammation.
In this prospective pilot study, 13 patients with long-standing IBD were prescribed cannabis treatment. The outcome was measured in quality of life. After 3 months treatment, patients reported improvement in the following areas:
- General health perception
- Social functioning
- Ability to work
- Physical pain
- Depression
Furthermore, cannabinoids also have an effect on appetite. Decreased appetite is a major factor for those with IBD, as ingestion of food often leads to pain, cramping and discomfort. This can also lead to fast and unintentional weight loss. The appetite stimulating effects of THC are applied in the case of chemotherapy patients, and there is no reason why it cannot be applied in the case of IBD patients.
With chronic conditions such as IBD, improving quality of life is one of the paramount objectives of treatment. There is no known cure for IBD, and pharmaceutical intervention mainly focuses on reducing inflammation and diarrhoea and managing pain. The reduction of debilitating symptoms such as these is crucial in maintaining a high quality of life, even in the presence of chronic conditions like IBD.
Dangers of long-term cannabis use in IBD
IBD is a chronic, long-term condition, and this is why the dangers associated with long-term use have to be discussed. To begin, IBD generally begins to express at around age 20, which poses a caveat for young people whose brains are still developing. Furthermore, adolescents (aged 18-20) who have IBD are unlikely to discuss their marijuana use with their gastroenterologist, meaning it is an important avenue of discussion for physicians themselves.
Another medical aspect to be considered for those with IBD is pregnancy. The jury is out with respect to using cannabis during pregnancy, but there is the possibility of complications.
Long term cannabis use in IBD patients may also have dire effects on gut permeability. Even though FAAH inhibitors showed promise in the treatment of IBD, there is also a risk, after long term use, of unfavourably affecting gut leakiness.
Finally, IBD is often accompanied by comorbidities such as cardiovascular disease. Those who have comorbidities should consider those conditions before medicating with cannabis.
The efficacy of cannabis in treating IBD is still being investigated, as scientific research in this area continues to develop. For the medical community to better understand exactly what role cannabis has to play in either the management of symptoms or the treatment of the disease, many more human trials need to be conducted. With all of that in mind, the research shows extreme promise.
- Disclaimer:This article is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your doctor or other licensed medical professional. Do not delay seeking medical advice or disregard medical advice due to something you have read on this website.











I find at times when symptoms are bad and I feel nauseated marijuana just makes it worse. But if it’s just my stomach and no head problems sometimes I find that weed doesn’t really effect it better or worse
I have diviticulitus. Whenever I smoke weed (or have oil) I get lots of pain in the side and end up having to take antibiotics. I use to smoke all the time, but now, just one small puff is all it takes to give me weeks of pain. It’s horrible.
I have just recently found out i have IBS. I thought i was dying of something. 3 months later and the symptoms are the same or worse than 3 months ago. I have started eating better and walking. I was using edible cannabis oil i made and thought it was causing the problem. When i quit taking it for 3 weeks the IBS was considerably worse.
It is anecdotal but cannabis relieves the symptoms and relaxes my stomach.
I have decided to take early retirement to reduce the stress and will continue with the diet excercise and cannabis approach.
The weight i have lost is already making most of me feel better…but my guts are yuck.
I believe for my situation cannabis really helps make it easier to cope with IBS and the cramps and pain.
I was recently diagnosed by my doctor with IBS, I have used Cannabis for 6 years now to help sleep and or have an appetite when stressed or anxious. In the last three days I used cannabis at night to sleep. Within a half hr of using it my IBS got literally painful, extremely painful. I thought my appendix was rupturing, for me Cannabis seems to be causing digestive problems. I’m confused as most people seem to think it helps and for me it has triggered it. I am positive the cannabis caused this as I’ve been eating the same food every day at the same time, a strict routine and only when I use Cannabis did I get cramps, bloating and discomfort. I confirmed this by changing how much Cannabis I used each night, the more I used the worse the cramps got.
Risto, how do you use your cannabis? I have found that smoking it in any way aggravates my IBS and inflammation. I have been making my own cannabis butter, using a strain that is a 1 to 1 ratio of THC and CBD, which really help to decrease the pain and inflammation. I also ensure the edibles (cookies) I prepare don’t contain the foods which upset my stomach. Hope this helps.
5:00am and sitting on the toilet suffering another bout of IBS. I knew this was a risk when I ate that Indian food last night… but it was sooo good. Anyway, here I am, and googling to see if a little THC would help. Going to try it and see, but surprised how little research is available.
Incredibly. The first half of the story is how I copied my life. I have recovered despite all the vices in my life. I do not hesitate to reach for a CDS solution of chlorine dioxide for every problem. It cured all my health problems, returned my appetite for life.
I have sufferd from terrible stomach problems that seem to have been caused originally through really bad binge drinking sessions, for over 10 years undiagnosable problems iv had telescopes shoved down my throat into my stomach, very unpleasant I can tell you and still they found nothing. ihave to smoke cannabis to relive my sickness.