Self-medication with cannabis is becoming increasingly popular with Parkinson’s disease patients. In fact, it is the prevalence of self-medication that has inspired scientific study to begin. However, some studies put forward conflicting results. Overall, many patients report relief from a multitude of symptoms after using medical cannabis.
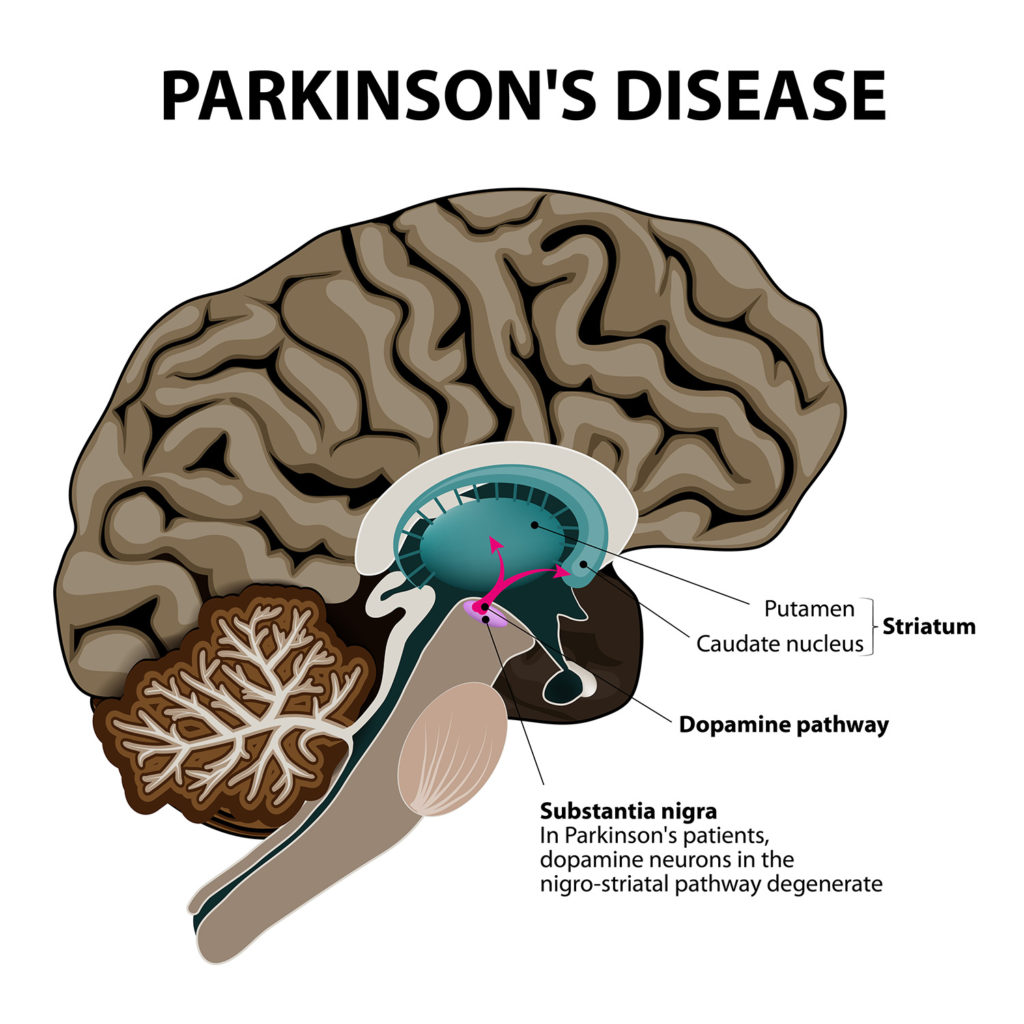
Parkinson’s disease is a neurodegenerative disorder that affects the central nervous system by causing the destruction of the dopamine-producing cells in an area of the brain known as the substantia nigra. The motor functions are first to be affected and as the disease progresses, cognitive decline, dementia and depression can take hold.
Stories of the-self medicated have inspired research into the use of cannabinoids to treat Parkinson’s disease. Many report having used cannabis oil as a means to manage symptoms of Parkinson’s, and since this information became the knowledge of the scientific community, more research has been conducted into the effects of THC and CBD on the symptoms of Parkinson’s.
What is Parkinson’s disease?
One of the main symptoms of Parkinson’s disease is a deterioration of motor functions, which can be grouped into 3 main symptoms: involuntary shaking of parts of the body (tremor), slow movement and stiff muscles. Tremors are certainly the most visible and well-known of the motor symptoms, but there are numerous other specific motor symptoms that patients can suffer from, depending on the individual.
In addition to the motor symptoms, there are also neuropsychiatric symptoms of Parkinson’s disease that can include a deterioration of certain cognitive functions, mood disorders or behavioural disorders. These disorders largely manifest themselves as problems with concentration, memory, language and visuospatial skills. The progressive deterioration of this cognitive capacity can, over the long-term, result in a much more severe manifestation of dementia.
Since the 1970s, the scientific community – prompted by frequent reports from patients opting for self-medication – has been able to focus its research on cannabinoids for the treatment of Parkinson’s disease. The number of studies conducted on the subject continues to be relatively low, despite recent renewed efforts in this direction owing to the frequency of cases reported by patients suffering from the disease.
1. Cannabis may be antidyskinetic
Dyskinesia is a common symptom of Parkinson’s disease. The term refers to involuntary movements of the muscles. Symptoms may manifest as uncontrolled twitching or shaking, progressing to extremely slow (or even total lack of) movement.
In Parkinson’s patients treated for prolonged periods with Levodopa (a naturally-occurring precursor to dopamine, which increases dopamine levels in the brain), a specific form known as Levodopa-induced dyskinesia can occur. This form can cause chorea (“dancing” movements of the feet and hands), dystonia (sustained muscular contractions leading to twisted, abnormal posture), ballism, myoclonus, or a combination of any of these.

The cannabinoid receptors of the central nervous system are densely clustered in an area of the substantia nigra known as the pars reticula, an area that is fundamentally involved with dopamine signaling to the striatum of the basal ganglia. The basal ganglia region is primarily responsible for the regulation of voluntary motor activity. Cannabinoid receptors are also present in high numbers in the basal ganglia themselves. Thus, the natural transmission of endocannabinoids is thought to play a role in these fundamental and related processes.
Various studies have indicated that agonization of the cannabinoid receptors by administration of exogenous cannabinoids may assist in the reduction of Levodopa-induced dyskinesia and other motor difficulties in Parkinson’s disease patients. A 2002 study on non-human primates concluded that this was indeed the case, as did a 2007 study on rats that utilized the synthetic agonist WIN 55,212-2.
However, studies on humans have proved inconclusive thus far. A small clinical trial of seventeen individuals conducted in the UK in 2004 concluded that there was no objective or subjective improvement in dyskinesia (levodopa-induced). In contrast, a 2014 observational study of twenty-two patients indicated improvements in tremor (shaking), rigidity and bradykinesia (slow movements).
2. Cannabis for anti-apoptosis
Abnormal apoptosis of dopamine-producing neurons in the pars compacta (the other main subdivision of the substantia nigra) is thought to be the primary mechanism of Parkinson’s disease. It is not known precisely how this phenomenon occurs, but it has been repeatedly demonstrated that treatment with dopamine receptor agonists can have beneficial effects, as they make up for the loss of neurons by stimulating the remaining ones to produce extra dopamine.
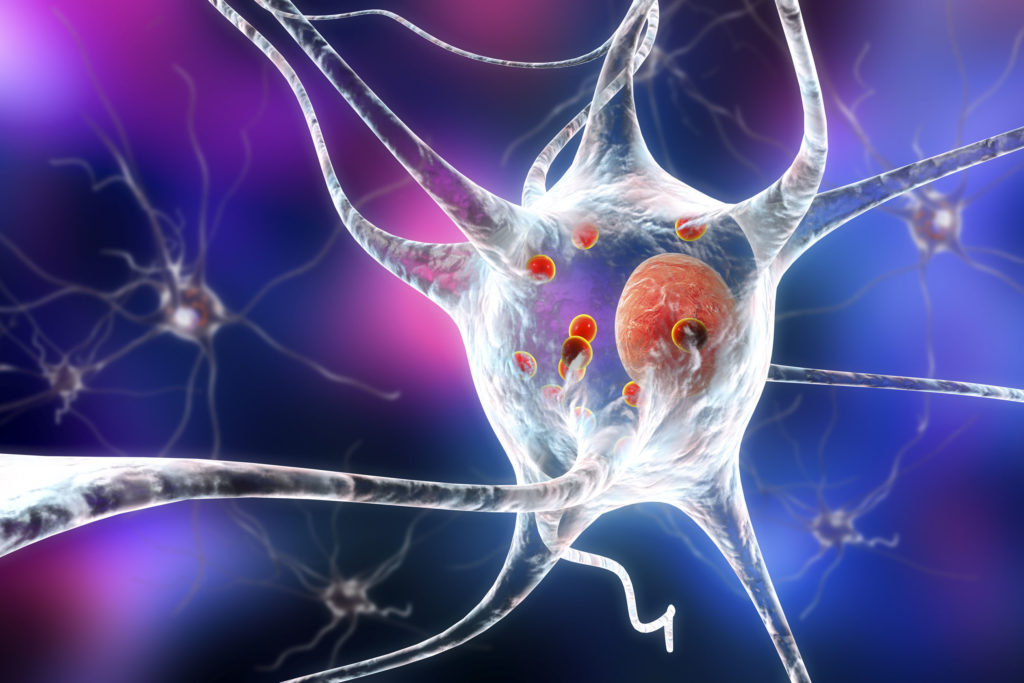
The endocannabinoid system is known to be heavily involved with the regulation of the natural processes of apoptosis—a form of controlled cell death that is a fundamental part of normal metabolic function. In some cases, cannabinoids have been shown to induce apoptosis (for example, in several forms of cancer), but there is also evidence that they can exert a protective effect and reduce excessive rates of apoptosis in certain diseases.
It is hypothesized that Parkinson’s disease may occur due to presence of a compound known as oxidopamine, which differs slightly in structure from dopamine in that it also contains a hydroxyl group (-OH). Its structural similarity allows it to be transmitted to the pars compacta via the dopamine reuptake transporters, whereupon it systematically destroys the dopaminergic (dopamine-producing) neurons.
A study published in 2005 demonstrated that injection of oxidopamine into the brains of mice led to a sharp reduction in dopamine levels, and that administration of delta-9-THC, CBD and the non-selective synthetic cannabinoid HU-210 exerted a permanent neuroprotective effect.
The fact that CBD had this effect indicates that the mechanism is dependent on the CB2-receptors (as CBD has negligible affinity for the CB1-receptor), which mediate the anti-inflammatory effects of the compounds and preserve cells from excessive apoptosis.
3. Cannabis as a sleep aid
Patients of Parkinson’s disease often have sleep-related issues, which can negatively affect the immune system and reduce patients’ capacity to fight off its progression. The disease usually affects older individuals, who often experience insomnia even if they do not suffer from Parkinson’s itself.
Indeed, the insomnia experienced by sufferers of Parkinson’s disease often differs from typical age-related insomnia. Parkinson’s patients usually have little difficulty in falling asleep, but have severe difficulty remaining asleep throughout the night, and in falling back to sleep if awoken. Some patients report increased incidence of nightmares and excessively vivid dreams, and some also report excessive daytime sleepiness.

Cannabis is well-known to induce sleep, and has been used to do since ancient times in various cultures. Furthermore, one of the primary symptoms of cannabis withdrawal in dependent users is insomnia. It is thought that both delta-9-THC and CBD have a role to play in the regulation of sleep. CBD specifically is thought to induce sleep, while delta-9-THC is believed to cause residual sedation (i.e. feelings of sleepiness subsequent to awaking). While this effect of THC may be disadvantageous for those suffering from excessive daytime sleepiness, it may assist in enabling patients with disrupted night-time sleep to fall asleep again.
4. Cannabis has antidepressant qualities
Up to 50% of individuals afflicted by Parkinson’s disease exhibit symptoms of depression, which can negatively affect disease progression in various ways. It is thought that there is a genetic contribution to the likelihood of Parkinson’s-afflicted individuals suffering depression. Polymorphisms of the CNR1 gene—which encodes for the expression of the CB1-receptors—may have a fundamental role to play.

A study published in Nature in 2005 indicated that individuals with a particular polymorphism consisting of two long-chain alleles in the CNR1 gene were less likely to develop depression as a symptom of Parkinson’s disease. It was also noted that depression was more likely in patients with akinetic Parkinson’s (rigidity and loss of movement) than in those with tremoric or mixed-type Parkinson’s.
Furthermore, various studies have indicated that depression is often accompanied by changes in levels of endogenous levels of cannabinoids such as anandamide and 2-AG in the prefrontal cortex, an area heavily involved in mood-regulation and decision-making.
While more research must be done to ascertain the precise relationship between Parkinson’s disease, CNR1 expression and depression, there is definite therapeutic potential in manipulation of the endocannabinoid system to reduce symptoms of depression in Parkinson’s-afflicted individuals.
5. Cannabis for pain management
The discovery of pain as a symptom of Parkinson’s disease is relatively recent. Even though musculoskeletal pain is the most common form, accounting for 40%–90% of the reported cases, it had not previously been linked to the disease in any conclusive way. However, this pain is often severe to the point of surpassing the other symptoms in terms of severity, and it can have psychological repercussions in the long term such as depression and anxiety.
Pain can be a direct consequence of the motor disorders, such as pain suffered as a result of prolonged muscle rigidity, or even pain linked to dystonia, postural problems, and more rarely, coming directly from the cervical region.

This 2012 study published in the European Journal of Pain was able to examine 12 different genes known to be involved with pain in general in a group of 229 Parkinson’s disease patients. The researchers then discovered that these genes reacted to pain in a recognisable way. Specifically, FAAH was associated with Parkinson’s disease-related pain, which is interesting because FAAH is an enzyme that metabolizes endogenous cannabinoids, including anandamide.
The researchers have recommended continued research in order to optimise potential treatment based on the individual characteristics of the patients’ gene mapping.
The one thing modern science can confirm with respect to this topic is that further research is warranted in the treatment of Parkinson’s with cannabinoids. Most preclinical studies point towards cannabis’ potential, and propose a foundation for the need to do more research in this field.
- Disclaimer:This article is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your doctor or other licensed medical professional. Do not delay seeking medical advice or disregard medical advice due to something you have read on this website.












Bonjour mon père vient d’être diagnostiqué il atteint de la parkinson la quelle exact a voir il doit faire des examens plus approfondis je suis consamateur régulier et je sais que le cannabis peut soulager/atténuer les tremblements j’aimerais savoir qu’elle et la meilleure variété pour cette maladie
I am now 59. With the new herbal medicine for Parkinson I purchased from Multivitamincare . org was my only way to get rid of my PD,the herbal formula effectively reversed my condition and alleviated all my symptoms, people are suffering from this Parkinson disease due to lack of information.
I am looking for help for my 53 year old son who has Parkinsons Desease. He is a medication and I would like to know if he has to get off of that medication or can he take cabannabis oil in addition to his meds.
Thanks, Richard
Dear Richard,
Thank you for your comment. We are sorry to hear about your situation. Unfortunately, as Sensi Seeds is not a medical practice, we are not able to provide any advice relating to medical situations other than to consult your doctor or other licensed medical professional. This article, written specifically for healthcare providers who may not be aware of the many properties of cannabis, may be useful to you in talking with your doctor. You could also try to contact local medicinal cannabis support groups, if you have not already done so. In the UK, there is the United Patients Alliance (you can find them on Facebook) and in the US and EU there are many branches of NORML (google NORML followed by your area name). We hope this is helpful.
With best wishes,
Scarlet
My oldest son has the early stages of Parkinsons desease. I would like to think this cannabis oil would help him. Looks good but I still have questions about Cannabis oil.
Is there any add’l info (recent) regarding Cannabis for Parkinson’s? I live in Colorado and personally derive a lot of benefit. My Young Onset PD group meets next week with this as a (still) controversial topic. I’d love to share any/all data you have.
Thanks!
Nancy Ivankoe
nivankoe@gmail.com